Mini Review 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Effects of Different Delivery Methods on The Functional Status of The Postpartum Pelvic Floor and Guidance on Pelvic Floor Rehabilitation Training
*Corresponding author:Li Xia, Hohhot Maternity and Child Health Care Hospital, Hohhot Inner Mongolia, China.
Received:April 06, 2023;Published:April 18, 2023
DOI: 10.34297/AJBSR.2023.18.002490
Abstract
Objective: This study is to investigate the effects of normal and cesarean delivery on the pelvic floor function of pregnant women in the early postpartum period. Methods: 277 pregnant women who delivered in our hospital were divided into two groups: normal delivery and cesarean delivery, and pelvic floor muscle function testing was performed at 42 d after delivery to compare the functional status of the pelvic floor in the two groups. Results: The overall score of the cesarean delivery group was higher than that of the normal delivery group; among the indicators, the incidence of abnormal pelvic floor muscles in the pre and post resting stages was higher in the cesarean delivery group than in the normal delivery group, and the incidence of abnormalities in the fast and slow muscle stages and the endurance test stage was lower than that in the normal delivery group, and the differences were statistically significant (p<0.05). Conclusion: Although cesarean delivery could reduce the incidence of early pelvic floor muscle abnormalities, postoperative pelvic floor muscle function and life would still be affected to a certain extent, and early instruction of pelvic floor rehabilitation training for pregnant women was beneficial to the recovery of pelvic floor function.
Keywords: Caesarean, Normal delivery, Pelvic floor function, Rehabilitation training
Introduction
The pelvic floor is composed of muscles, ligaments and fascia that support the pelvic organs such as the bladder, genitals and rectum [1]. Pelvic Floor Dysfunction (PFD) occurs most often in women after childbirth and is closely related to damage to the supporting structures of the pelvic floor [2]. The female pelvic floor, as a muscle group supporting important pelvic organs, has a very important role in protecting women from stress urinary incontinence [3], vaginal wall bulge [4], uterine prolapse, and other diseases [5]. Many factors influence PFD, and some studies have reported that the pelvic floor muscles are subject to continuous stretching and tearing and thus relaxation during pregnancy and childbirth, making them two independent risk factors for PFD [6]. Currently, biofeedback combined with electrical stimulation therapy [7] is commonly used clinically to treat PFD and to guide pregnant women to perform pelvic floor rehabilitation training. In this study, pelvic floor function was tested by 277 postpartum pregnant women in our hospital. The postnatal resting state muscle tone, fast and slow muscle contraction force and endurance were used as evaluation indexes to analyze the effect of delivery mode on the postnatal pelvic floor function condition of pregnant women, and to suggest pelvic floor rehabilitation training for patients with pelvic floor abnormalities in order to protect women's physical and mental health and postnatal quality of life, and to provide theoretical basis for the prevention and treatment of PFD.
Materials and Methods
General Data
277 women who delivered in our hospital from February to October 2021 and underwent pelvic floor function testing at 42 d postpartum were selected as study subjects. The control group was delivered by cesarean section with 107 cases and the average age was (30.2±5.1) years; the observation group was delivered vaginally with 170 cases and the average age was (30.3±5.5) years, and the general data of the two groups were comparable with no statistical significance (p>0.05).
Inclusion and Exclusion Criteria
Inclusion criteria: All were women who underwent delivery in our hospital, full-term singleton, without inflammatory symptoms such as vaginal bleeding and edema, and patients were informed and agreed to participate in this study.
Exclusion criteria: Patients with pre-pregnancy diseases such as urinary incontinence, previous pelvic surgery or pelvic floor rehabilitation treatment.
Methods
In this study, the neuromuscular stimulation therapy instrument(MLD B4 Medlaner, Nanjing, Jiangsu, China) was used to measure the pelvic floor function in postpartum pregnant women [8]. was used to measure the pelvic floor function in postpartum pregnant women. The procedure was as follows: the bladder was emptied, the pregnant woman was instructed to be in a supine position, relaxed, with the knees separated at shoulder width, the perineum was exposed, and the electrode pad site was disinfected. The electrode was then fixed and the instrument probe was extended to 5cm into the vagina, and muscle contraction and relaxation were performed according to the requirements of the instrument to test the anterior and posterior resting states, the fast and slow muscle phases and the endurance test phase of the pelvic floor muscle. The assessment indexes included the overall score, the mean value of the anterior resting phase (reference value <4 μV), the mean value of the fast muscle contraction (reference value >40 μV), the mean value of the slow muscle contraction (reference value >35 μV), the mean value of the endurance test (reference value >30 μV), and the mean value of the posterior resting phase (reference value <4 μV).
Statistical Methods
SPSS 23.0 software was used to process and analyze the data. The measurement data were expressed as mean ± standard deviation (±S), and t-test was used for comparison between groups. Count data were expressed as percentages (%), and the chi-square test was used for comparison between groups, and differences were considered statistically significant at p<0.05.
Results
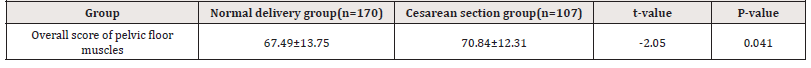
1. Comparison of pelvic floor muscle function scores between two delivery methods at 42 d postpartum
The average score of pelvic floor muscle at 42 d after delivery was 67.49 in the cesarean group and 70.84 in the cesarean group, and the total score of the cesarean group was significantly higher than that of the cesarean group, and the difference was statistically significant (p<0.05) (Table 1).
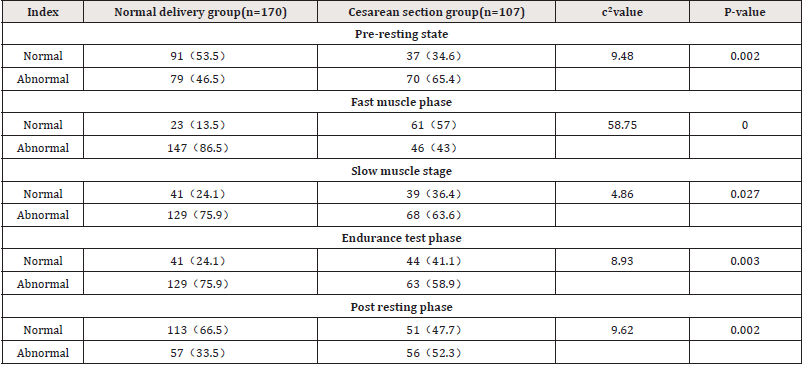
2. Comparison of the incidence of pelvic floor muscle abnormalities at each stage between the two delivery methods
The pelvic floor function of pregnant women at each stage of the two delivery methods is shown in Table 2.The incidence of pelvic floor muscle abnormalities in the anterior resting and posterior resting states was higher in the cesarean group than in the cesarean group, and the difference was statistically significant (p<0.05); the incidence of pelvic floor abnormalities in the fast muscle, slow muscle and endurance test stages was higher in the cesarean group than in the cesarean group, and the difference was statistically significant (p<0.05) (Table 2).
Discussion
The pelvic floor muscles, as the muscle groups that support the pelvic organs, are important parts of the body that ensure the smooth functioning of the female organism such as excretion. During pregnancy and childbirth, the muscles in the pelvic cavity are stretched to varying degrees, while under the influence of hormones and the fetus, the pelvic floor muscles can cause certain damage, which in turn can lead to different degrees of pelvic floor dysfunctional diseases [9,10]. Therefore, it is of great importance to pay attention to the pelvic floor function of postpartum women, to perform pelvic floor muscle strength testing as early as possible, and to instruct them to perform pelvic floor rehabilitation training in abnormal cases to ensure the physical and mental health of pregnant women after delivery.
This study evaluated the pelvic floor function of pregnant
women in the early postpartum period by detecting five indicators
including resting muscle tone using the neuromuscular stimulation
therapy instrument(MLD B4, Medlaner, Nanjing, Jiangsu, China).
The specific significance includes the following:
1) The anterior resting phase mainly focuses on static pelvic
floor muscle tone, and when the average value >4 μV indicates
elevated resting pelvic floor muscle tone, there is a risk of pelvic
floor muscle ischemia, painful intercourse, urinary retention and
constipation.
2) The fast muscle stage mainly monitors the muscle
strength and reaction speed of dynamic class II muscle fibers, and
when the muscle strength is insufficient, it will cause incontinence,
sexual incoordination, and other related problems.
3) The slow muscle phase mainly observes the dynamic class
I muscle fiber muscle strength and contraction control stability in
pregnant women, and weaker muscle strength can cause stress
urinary incontinence, pelvic organ prolapses and defecation
dysfunction and other risks [11].
4) The endurance test phase mainly tests the endurance
of the pelvic floor muscles, and a lower mean value indicates a
decrease in pelvic floor muscle endurance.
5) Post resting phase mainly tests the static pelvic floor
muscle tone, when the mean value measured >4 μV, it indicates
elevated resting tone and predisposition to constipation and other
diseases.
The pelvic floor muscle strength was measured in pregnant women who delivered vaginally and by cesarean section, and the results showed that the mean value of muscle tone in the anterior and posterior resting phases was significantly higher in the cesarean section group than in the normal delivery group (p<0.05). The pelvic floor muscle tone was generated by the mutual traction of muscle cells, and for pregnant women who delivered by cesarean section, the fetus in the uterus would exert pressure on the pelvic floor muscles, causing pelvic floor muscle relaxation, and after the release of the pressure after delivery, the vagina was in a state of fatigue, and there was an increase in reactive muscle tone, which might be one of the reasons why the muscle tone of pregnant women who delivered by cesarean section was higher than that of pregnant women who delivered by normal delivery. At the same time, the fetus was not delivered vaginally, and the vaginal muscles were therefore less mobile, resulting in the brain center not receiving negative feedback regulation of the muscles, which also resulted in the inability of the pelvic floor muscles to relax and thus higher muscle tone [12,13].
The results of the study also showed that the incidence of abnormalities of the pelvic floor muscles in the fast, slow and endurance test phases was higher in the cesarean group than in the cesarean group, indicating that the cesarean delivery method had less adverse effects on the function of the pelvic floor muscles in pregnant women. But pregnant women who delivered vaginally were more likely to suffer from incontinence, pelvic organ prolapse and defecation dysfunction [14,15]. In women who deliver vaginally, the fetus dilates during vaginal passage and the surrounding muscles and fascia were stretched and damaged, resulting in the inability of the pregnant woman to contract the pelvic floor muscles normally on her own and poor coordination of the pelvic floor muscles, which led to PFD [16]. Although vaginal delivery was more damaging to the pelvic floor, it was not encouraged to perform cesarean section, which was associated with the risk of intraoperative infection, inflammatory reaction, and postoperative complications, and also caused some medical damage to the pelvic floor [17]. Therefore, early detection of pelvic floor muscle function in postpartum pregnant women, analysis of the influencing factors, and guidance of pelvic floor rehabilitation training for different conditions were effective means to ensure a healthy postpartum pelvic floor and life of pregnant women [18].
Our hospital used neuromuscular stimulation therapy instrument to test the pelvic floor muscle function of postpartum
Acknowledgments
None.
Conflict of Interest
None.
References
- Eickmeyer SM (2017) Anatomy and Physiology of the Pelvic Floor. Phys Med Rehabil Clin N Am 28(3): 455-460.
- Jörgen Quaghebeur, Peter Petros, Jean Jacques Wyndaele, Stefan De Wachter (2021) Pelvic-floor function, dysfunction, and treatment. Eur J Obstet Gynecol Reprod Biol 265: 143-149.
- Kobra Falah Hassani, Joanna Reeves, Rahman Shiri, Duane Hickling, Linda McLean (2021) The pathophysiology of stress urinary incontinence: a systematic review and meta-analysis. Int Urogynecol J 32(3): 501-552.
- Bureau M, Carlson KV (2017) Pelvic organ prolapse: A primer for urologists. Can Urol Assoc J 11(6Suppl2): S125-S130.
- Eickmeyer SM (2017) Anatomy and Physiology of the Pelvic Floor. Phys Med Rehabil Clin N Am 28(3): 455-460.
- Xu T, Liu KS, Luo HH (2023) Research progress of physiotherapy in women with pelvic floor dysfunctional diseases. J Repr Med 32(2): 296-300.
- Xiaoli Wu, Xiu Zheng, Xiaohong Yi, Ping Lai, Yuping Lan (2021) Electromyographic Biofeedback for Stress Urinary Incontinence or Pelvic Floor Dysfunction in Women: A Systematic Review and Meta-Analysis. Adv Ther 38(8): 4163-4177.
- Mo CHM, Lai M, Deng LCH (2016) Clinical efficacy of PHENIX neuromuscular stimulation therapy instrument with pelvic floor rehabilitation device in the treatment of female pelvic floor dysfunctional diseases. Practical Integrative Chinese and Western Medicine Clinical 5: 28-29.
- Song TJ, Zhao LJ, Wang Y (2021) Influencing factors of pelvic floor dysfunction in women and progress of rehabilitation treatment. China Maternal and Child Health Care 2: 479-482.
- Blomquist JL, Carroll M, Muñoz A, Handa VL (2020) Pelvic floor muscle strength and the incidence of pelvic floor disorders after vaginal and cesarean delivery. Am J Obstet Gynecol 222(1): 62.e1-62.e8.
- Wang SN, Huang HJ (2017) Analysis of postpartum pelvic floor muscle strength situation and influencing factors. Southeast Defense Medicine 02: 121-125.
- Li JY, Wu JP, Lai HC, et al. (2019) Effect of delivery mode differences on postpartum pelvic floor muscle strength. Modern Hospital 19(02): 290-291+294.
- Dilibaier Anwaier, Liu N, Gulina Ababaykli (2018) Effect of different delivery methods on pelvic floor muscle strength in the early postpartum period. Journal of Xinjiang Medical University 06: 692-696.
- Wenguang Yan, Xuhong Li, Shaodan Sun, Yali Xiang, Yanhua Zhou, et al. (2018) Risk factors for pelvic organ prolapse and urinary incontinence in women. Journal of Central South University (Medical Edition) 43(12): 1345-1350.
- Liu W, Liu P, Wang YX (2019) Effects of different degrees of perineal laceration on pelvic floor function during vaginal delivery in primiparous women. Chinese Family Planning and Obstetrics and Gynecology 12: 50-53.
- Shen Y (2021) Investigation of factors influencing early postpartum recovery of pelvic floor muscle function in primiparous women with transvaginal delivery. General Practice Nursing 04: 546-549.
- López López AI, Sanz Valero J, Gómez Pérez L, Pastor Valero M (2021) Pelvic floor: vaginal or caesarean delivery? A review of systematic reviews. Int Urogynecol J 32(7): 1663-1673.
- Martin Huser , Petr Janku , Robert Hudecek , Zuzana Zbozinkova , Miroslav Bursa et al. (2017) Pelvic floor dysfunction after vaginal and cesarean delivery among singleton primiparas. Int J Gynaecol Obstet 137(2): 170-173.
- Shi JM, Zhang Yi (2021) Research progress of vaginal dumbbell in the treatment of female stress urinary incontinence. International Journal of Obstetrics and Gynecology 48(02): 208-212.
- Liu LM, Huang HY, Cai LY (2020) Effect of Kegel exercise method combined with biofeedback electrical stimulation on the effect of postpartum pelvic floor rehabilitation management. Guangzhou Medicine 03: 42-46.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.